In 2024, ransomware attacks disrupted hospital systems across 46 U.S. states. Some providers lost more than $100 million per day due to billing freezes, while others were forced to revert to handwritten charts and manual medication logs, which led to near-misses involving infant dosing errors. One of the nation’s largest healthcare systems, Ascension, suffered outages so severe that patients were rerouted, diagnostic results were delayed, and safety checks were missed entirely. And yet, there is still no mandatory federal hospital cybersecurity framework in place to prevent similar events from recurring tomorrow.
Hospital cybersecurity is no longer just a back-office concern; it has become an urgent public health issue. A staggering 92% of healthcare organizations reported cyberattacks in the past year alone, up from 88% the year before. These attacks aren’t just stealing data; they are delaying cancer treatments, halting surgeries, and contributing to increased mortality. The combination of outdated IT infrastructure, underfunded cybersecurity programs, and lax regulatory oversight has created the perfect storm, leaving patients directly in harm’s way.
This post explores the structural failures behind the ongoing crisis in hospital cybersecurity. Drawing on recent breaches, expert data, and real-world hospital impacts, we’ll break down what’s gone wrong, what the consequences have been, and what actionable steps hospitals, policymakers, and the public must now take. Each section will address a distinct part of the problem, ranging from ransomware attacks on hospitals and healthcare data breaches to medical device vulnerabilities and systemic failures in hospital network security.
We cover stories like this every week at Quantum Cyber AI. If you want detailed breakdowns of the cyber threats shaping our health systems and democracy, subscribe to our newsletter here.
Before we can address the solutions, we need to understand just how widespread and systemic the hospital cybersecurity crisis has become.
Why Hospital Cybersecurity Is a Growing Crisis
The Alarming Surge in Attacks

Hospital cybersecurity has reached a tipping point. In 2023, record-breaking levels of healthcare data breaches were reported, with ransomware attacks accounting for nearly 33% of all incidents. These aren’t just isolated events; they reflect a systemic vulnerability that threat actors continue to exploit with precision. From local clinics to multi-state providers, no institution is immune.
The frequency of ransomware attacks on hospitals has risen by 300% since 2015, according to IBM’s global threat reports. These attacks have increasingly targeted mission-critical hospital operations, including patient records, imaging systems, pharmacy databases, and scheduling platforms. The result is a sustained disruption in care delivery, all while attackers demand multimillion-dollar payments in cryptocurrency.
Vulnerable Infrastructure and Underfunding
Many hospital networks still rely on legacy infrastructure, with outdated operating systems, unsupported software, and decentralized access control systems. According to the American Hospital Association, even large providers are often burdened by underfunded IT departments unable to keep pace with evolving threat vectors.
Medical device vulnerabilities further compound the threat. MRI machines, infusion pumps, and diagnostic sensors are frequently connected to hospital networks without proper segmentation or encryption. A study from arXiv found that IoT medical devices in hospitals are “routinely exposed to unauthorized scanning, outdated firmware, and insecure remote access protocols.”
These weak points allow threat actors to move laterally once inside the network, escalating from one compromised endpoint to full-system lockdowns. Worse still, many hospitals have no formal incident response plans, no offline backups, and no dedicated cybersecurity leadership. This makes recovery slow and patchy even after breaches are discovered.
The Cost of Inaction
The financial toll of hospital cyberattacks is enormous, but the human cost is even greater. Still, financial losses are driving attention at the federal level. Last year, the U.S. government proposed over $9 billion in new cybersecurity investments for hospitals, recognizing the scale of devastation caused by breaches that have impacted nearly 167 million Americans in the past decade.
Perhaps the clearest example of the cost of inaction is the Change Healthcare breach in February 2024. The attack disrupted billing and prescription operations at scale, leaving some hospitals unable to process insurance claims, fill prescriptions, or schedule procedures. Industry-wide losses reached into the billions, and many small providers were forced to furlough staff or halt services altogether.
In a healthcare environment increasingly reliant on digital infrastructure, failing to invest in hospital cybersecurity isn’t just negligent; it’s dangerous. Behind every statistic is a real-world consequence, and when hospital systems fail, it’s patients who suffer the most.
The Human Cost of Ransomware in Healthcare
Delayed and Denied Medical Care
When ransomware attacks on hospitals strike, the most immediate victims are not the IT departments; they are the patients. One of the most harrowing examples unfolded in 2024, when Ascension Health, which operates over 140 hospitals across the United States, suffered a massive cybersecurity breach. The attack forced care teams to switch to handwritten documentation, delayed lab results, and introduced errors in medication and surgical planning. According to NPR, nurses at multiple locations reported near-misses involving pediatric dosing and missed safety checks due to system downtime.
This is not an isolated case. As ransomware attacks on hospitals become more targeted and sophisticated, care delivery delays are growing longer and more dangerous. In many cases, emergency rooms have been forced to reroute incoming ambulances, cancel elective surgeries, and shut down critical systems like radiology and pharmacy databases. These disruptions point to an alarming breakdown in hospital network security, where systems that should be redundant or isolated are instead completely crippled by a single point of failure.
In a digital-first healthcare system, cybersecurity is care infrastructure. When hospital cybersecurity fails, so do diagnoses, treatments, and surgical outcomes.
Increased Patient Mortality
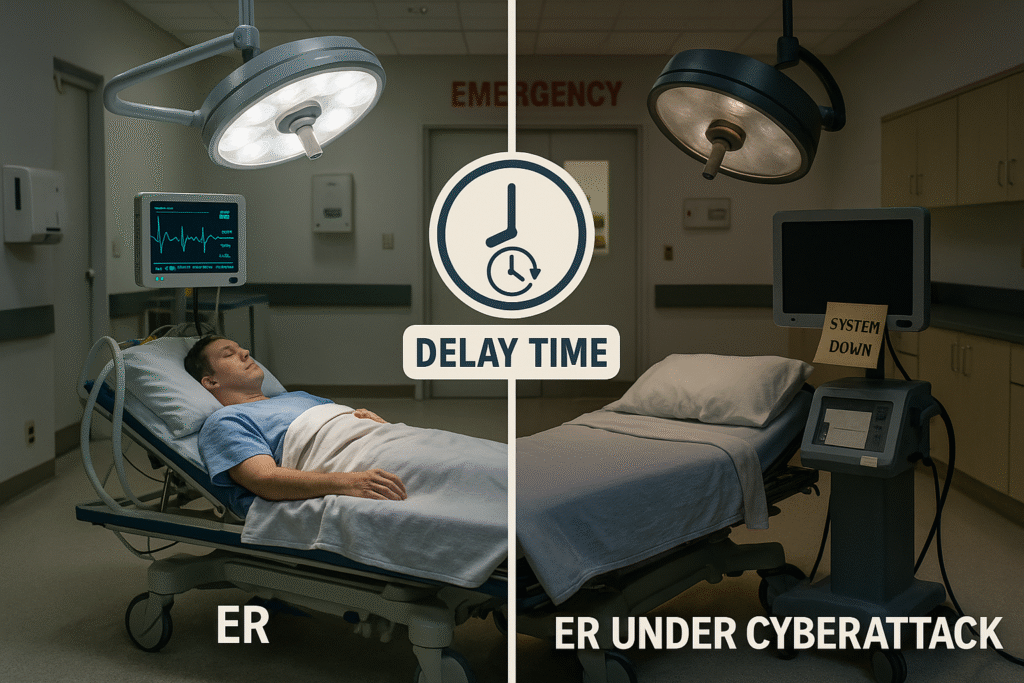
While the human cost of ransomware attacks on hospitals often feels intangible, the data paints a sobering picture. A peer-reviewed study published on arXiv linked healthcare data breaches to a 0.338 to 0.446 percentage point increase in 30-day mortality following heart attacks. That margin of error may sound small, but it reverses an entire year’s worth of improvements in patient outcomes nationwide.
IBM’s threat intelligence team has also documented a direct correlation between ransomware incidents and increased rates of cardiac arrest in nearby hospitals. In one instance, a hospital under attack had to shut down its emergency department, causing surrounding facilities to absorb the overflow. As a result, response times increased, and more patients died during transport or shortly after arrival.
Healthcare systems are designed to operate in tight, coordinated units. When hospital network security is breached, those units fragment and create chaos across entire metropolitan areas.
Psychological and Ethical Fallout
The emotional toll on medical staff and patients during ransomware attacks is often overlooked but just as critical. At Ascension, frontline providers described working in a constant state of crisis, unsure whether patient records were complete or medications had been safely administered. Many reported moral distress, fearing that decisions made under these conditions could cause harm.
For patients, the psychological burden is equally severe. Being transferred mid-treatment, losing access to test results, or witnessing hospital chaos undermines trust in the institution. These effects are compounded when healthcare data breaches expose personal health information, creating lasting anxiety over identity theft and privacy loss.
Medical device vulnerabilities add another layer of ethical complexity. Devices such as insulin pumps and heart monitors are increasingly connected to hospital networks but often lack security safeguards. If compromised, these tools can deliver the wrong dosage or shut down entirely. When ransomware disables access to these systems, the consequences are not only technical; they are life-threatening.
This convergence of hospital cybersecurity failures, data breaches, and vulnerable infrastructure creates a perfect storm. Patients are harmed, staff are demoralized, and trust in the health system is eroded. And with AI-generated scams and deepfake-enabled infiltration now emerging as new tools in attackers’ arsenals, the threat landscape is only expanding. For more on how digital deception is being used to infiltrate critical systems, see our analysis of the North Korean deepfake job scam.
To fully grasp how hospital cybersecurity breaks down in practice, we need to look closely at some of the most devastating and preventable breaches in recent years.
7 Shocking Cybersecurity Failures in Hospitals
Change Healthcare (February 2024)
The ransomware attack on Change Healthcare may be the most damaging healthcare cyber incident in U.S. history. In February 2024, attackers crippled systems responsible for processing billions in insurance claims and managing pharmacy benefits. As one of the largest clearinghouses in the country, Change Healthcare’s disruption immediately affected hospitals, clinics, and pharmacies nationwide. More than 75% of hospitals in the U.S. reported direct or indirect impacts, with some providers losing over $100 million per day due to delayed reimbursements and frozen operations.
This event exposed the fragility of centralized third-party systems in hospital network security. Despite not being a care provider itself, Change Healthcare’s role was so deeply embedded in the ecosystem that its collapse paralyzed entire segments of the industry. The attack also highlighted the urgent need for mandatory cybersecurity standards that include vendors, not just frontline providers.
Ascension Health (May 2024)
In May 2024, Ascension Health, a system with 140 hospitals and over 40 senior care facilities, was hit by a ransomware attack that shut down electronic medical records, imaging, pharmacy, and lab systems. Providers were forced to revert to manual processes, including handwritten medication charts and surgical orders. This led to severe workflow breakdowns and, in at least one reported case, a near-miss involving infant medication dosing.
The incident underscores a dangerous reality: hospital cybersecurity failures are not just about lost data; they can directly threaten lives. When ransomware attacks on hospitals freeze critical systems, patients may be treated based on incomplete or outdated information, raising serious ethical and medical concerns.

Emsisoft Report (2023)
A comprehensive report by Emsisoft in 2023 found that 141 U.S. hospitals across 46 systems were hit by ransomware in a single year. In 32 of those cases, protected health information (PHI) was confirmed stolen. These attacks led to canceled outpatient services, delayed surgeries, and forced shutdowns of emergency departments.
The report paints a bleak picture of hospital network security: even with years of warnings, most institutions remain vulnerable to basic exploit techniques. It also confirms that healthcare data breaches are not only becoming more common but more invasive.
CrowdStrike Outage (July 2024)
In a surprising twist, not all hospital cybersecurity failures stem from external threat actors. In July 2024, a faulty security update from cybersecurity firm CrowdStrike inadvertently disabled systems across hundreds of hospitals worldwide. While not a malicious attack, the incident demonstrated how fragile hospital infrastructure can be when overly reliant on a single point of digital control.
Hospitals canceled procedures, delayed patient intake, and were forced back to paper workflows while systems were restored. The event illustrates the cascading effects of weak redundancy planning and highlights how even security tools themselves can create systemic risk when not thoroughly tested.
Alder Hey Children’s Hospital (November 2024)
In the UK, Alder Hey Children’s Hospital fell victim to a ransomware attack that compromised sensitive records from 2,254 patients. Though the hospital quickly isolated and shut down systems, the leaked data still ended up circulating online. As investigations unfolded, parents voiced deep concerns about long-term implications for their children’s privacy and safety.
This case is a sobering reminder of how medical device vulnerabilities and insufficient encryption of patient records can escalate into public crises. Pediatric care involves some of the most sensitive data collected in medicine. When hospital cybersecurity breaks down, these patients are left the most exposed and the least able to advocate for themselves.
DaVita Dialysis Clinics (April 2025)
DaVita, one of the largest providers of dialysis services in the world, confirmed a ransomware attack in April 2025 that impacted 2,605 clinics across the United States. While the company was able to activate contingency protocols and continue patient care, the scale of the breach was staggering. The attack demonstrated that even highly prepared organizations with distributed operations remain vulnerable when targeted systematically.
DaVita’s response also shed light on best practices: clear public communication, isolated backups, and rapid deployment of offline protocols helped mitigate worse outcomes. Still, the attack showed that hospital network security must be designed not only for prevention but for resilient continuity of care.
Ireland’s HSE (May 2021)
Although not a recent case, the 2021 ransomware attack on Ireland’s Health Service Executive (HSE) remains one of the most disruptive global examples of how ransomware attacks on hospitals can impact national health infrastructure. The breach halted nearly all IT operations for several weeks, leading to an 85% drop in cancer trial referrals and the cancellation of 513 therapy sessions.
The HSE incident emphasized how medical device vulnerabilities, lack of segmented networks, and absence of strong data recovery policies can paralyze an entire healthcare system. Years later, it is still cited as a case study in what happens when a national provider underestimates the threat of hospital cybersecurity failure.
These seven cases, each with its own operational and ethical failures, are not outliers. They are warnings. And if nothing changes, they will keep repeating. To understand why these devastating incidents keep happening, we need to examine the policy vacuum that has allowed hospital cybersecurity to remain dangerously underregulated.
Why Federal Policy Still Lags Behind
Patchwork of Inadequate Guidelines
Despite the severity of recent cyberattacks, there is still no binding federal hospital cybersecurity standard in the United States. HIPAA, the primary regulatory framework governing health data, was designed in the 1990s. While it includes provisions for data privacy and some technical safeguards, it does not account for modern cyberthreats like ransomware attacks on hospitals or coordinated attacks on network infrastructure. Even with updates, HIPAA lacks the enforcement mechanisms and real-time responsiveness needed to protect hospital systems from today’s adversaries.
In late 2024, the Biden administration proposed new cybersecurity rules aimed at hardening hospital defenses. These included mandatory multi-factor authentication (MFA), third-party audits, and tighter access controls. While a step in the right direction, these proposals remain voluntary or slow-moving in implementation. Critics argue that until these guidelines become enforceable, the gap between policy and practice will continue to widen.
Hospital cybersecurity cannot rely on recommendations alone. Without federal mandates, many facilities will continue to postpone investment in security upgrades, increasing their exposure to ransomware and data breaches.
Vulnerabilities in Third-Party Systems
The Change Healthcare incident showed just how vulnerable hospitals are to cyberattacks that originate outside their own systems. Although hospitals were not directly hacked, the collapse of a centralized vendor paralyzed their operations. This raises urgent questions about the scope of existing policies. Currently, federal standards rarely extend to third-party service providers, even when those vendors are critical to billing, pharmacy access, or patient recordkeeping.
This oversight leaves a massive blind spot in hospital network security. Hospitals may be compliant within their own systems but still be vulnerable due to the weak cybersecurity of their partners. Until vendors like claims processors, software providers, and cloud storage services are required to meet the same cybersecurity thresholds, hospitals will remain at risk by association.
Lawmakers and regulators must confront this structural gap. Without third-party accountability, even the best-prepared hospital can be brought down by an unsecured link in the chain.
Resource Inequality Between Large and Small Providers
Large hospital systems may have the budget to invest in cybersecurity teams, penetration testing, and staff training. Smaller and rural hospitals often do not. According to reporting from the Washington Post, many rural providers cannot afford even basic measures like endpoint detection systems or secure backups. Some still use unsupported software due to licensing costs.
This inequality means that national hospital cybersecurity readiness is only as strong as its weakest facilities. A ransomware attack on a small regional hospital may not make headlines, but the consequences for the local population can be severe. It may take weeks or months to restore services without external help.
Without federal funding earmarked specifically for hospital network security, many of these institutions will remain exposed. Proposals for grants or public-private partnerships exist but have yet to materialize at the scale needed.
Lack of Real-Time Threat Intelligence Sharing
Another critical gap is the lack of centralized systems for real-time threat intelligence across healthcare organizations. While sectors like finance and defense have institutionalized rapid threat-sharing protocols, most hospitals operate in isolation when under attack.
The American Hospital Association has called for a healthcare-focused threat exchange platform that would allow hospitals to alert one another in real time about emerging threats, indicators of compromise, and active intrusion vectors. Without it, hospitals often do not find out they are part of a broader attack campaign until the damage has been done.
This policy void is not just technical; it is strategic. If hospitals continue to operate as isolated targets, adversaries will keep finding success.
To prevent future breaches, hospitals must take proactive steps on their own. The next section explores concrete, immediate actions facilities can implement to improve their cybersecurity posture.
How Hospitals Can Strengthen Cyber Defenses Today
Patch Management and Device Updates
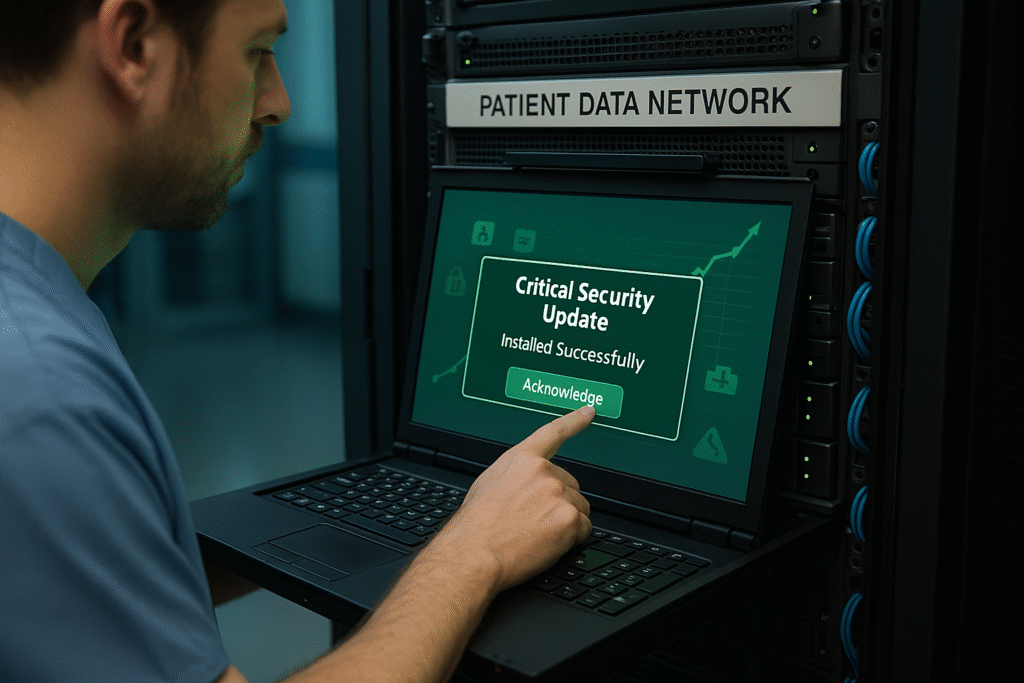
One of the most preventable causes of healthcare data breaches is unpatched software. According to cybersecurity research published in arXiv, approximately 32 percent of successful cyberattacks on hospitals exploit known vulnerabilities that were never patched. This includes operating systems, outdated antivirus programs, and third-party applications embedded across hospital systems.
Patch management is often deprioritized in healthcare settings due to concerns over downtime or compatibility with legacy equipment. However, delaying these updates creates open doors for ransomware attacks on hospitals. Automated patching systems, scheduled maintenance windows, and better IT-staff coordination can reduce the lag time between vulnerability disclosure and mitigation.
Cybersecurity hygiene is not optional. In hospital cybersecurity, basic system maintenance can be the difference between business continuity and a system-wide shutdown.
IoT and Medical Device Hardening
Modern hospitals are filled with internet-connected devices. From ventilators and infusion pumps to imaging systems and heart monitors, these tools improve care efficiency but also increase attack surface. Unfortunately, most medical devices were not designed with security in mind. They often lack encrypted communication, require default passwords, and cannot be updated easily.
A 2025 study from arXiv and additional reporting from Cybersecurity Ventures warn that these medical device vulnerabilities are now a primary vector for initial access by threat actors. Once attackers compromise one connected device, they can move laterally into hospital network systems.
Hospitals should isolate medical devices on segmented networks and deploy device monitoring systems that flag unusual traffic or commands. At a minimum, all IoT devices must be inventoried, assigned risk scores, and subject to routine penetration testing.
Staff Training and Incident Response Drills
Hospital staff are often the last line of defense during a cyberattack. Yet most healthcare workers receive minimal cybersecurity training, and even fewer participate in simulated incident response exercises. This lack of preparation has real consequences. When ransomware hits, miscommunication and panic often delay containment and recovery.
Programs such as Black Hat’s tabletop exercises have shown that realistic simulations dramatically improve staff response time and decision-making during live incidents. These drills help teams understand not just what to do but how to work together under pressure.
Hospital cybersecurity is a team sport. Training clinical staff, administrators, and IT personnel in shared response protocols is critical to minimizing downtime and preventing irreversible damage during an attack.
Vendor Risk Assessments and Cloud Security
While hospitals are starting to focus more on their internal systems, many still overlook the vulnerabilities introduced by third-party vendors. Cloud providers, data processors, and software platforms must also meet high security standards, but they often operate outside the direct control of hospital IT departments.
Hospitals must perform regular risk assessments on vendors, reviewing security certifications, breach history, and incident response readiness. Contracts should include cybersecurity clauses that require prompt notification of breaches, adherence to security standards, and joint response protocols.
Furthermore, hospitals using cloud-based systems should enforce access controls, encrypt all stored data, and require multifactor authentication for both staff and vendors. Hospital network security is only as strong as its weakest third-party connection.
These practical defenses can significantly improve resilience, but even the most prepared hospitals cannot solve the problem alone. To protect patients and restore trust, broader systemic action is needed, starting with demands from both the public and policymakers.
What Patients and Policymakers Must Demand
Encryption and Auditable Access Control
At the core of every hospital cybersecurity strategy should be encryption and access control. Despite years of recommendations, many healthcare facilities still fail to encrypt protected health information (PHI) at rest or in transit. Without encryption, healthcare data breaches expose sensitive patient records to anyone who gains access, whether intentionally or not.

Auditable access control is equally critical. Hospitals need to track who accesses patient records, when, and from which systems. This type of logging enables early detection of abnormal activity and supports investigations when incidents occur. The Biden administration’s 2024 policy proposals recommended mandatory multifactor authentication (MFA) and audit trails as baseline requirements, but these have not yet been universally adopted or enforced.
If hospitals continue to neglect these core protections, the consequences will not just be operational; they will be personal.
Mandatory Cybersecurity Standards for Critical Vendors
Patients and advocates should push lawmakers to close the vendor gap in hospital cybersecurity. When Change Healthcare was attacked, it was not a hospital that failed; it was a vendor. Yet the fallout affected millions of patients and hundreds of hospital systems.
Current regulations do not require most healthcare vendors to meet the same security standards as hospitals. This policy loophole leaves hospital network security exposed to third-party vulnerabilities. Lawmakers must expand the scope of regulation to include all vendors handling PHI, billing, imaging data, or infrastructure management.
Vendor accountability is not just a legal issue; it is a structural requirement for protecting care continuity and patient safety.
Greater Transparency and Breach Disclosure
One of the most frustrating realities for patients is how little they are told after a cybersecurity incident. In many cases, hospitals delay disclosure or provide vague updates that fail to explain the scope of a breach. This lack of transparency erodes public trust and prevents affected individuals from taking timely action to protect themselves.
Patients have the right to know when their records are compromised, how their care might be affected, and what is being done to fix the problem. Healthcare data breaches that impact millions of records should not be kept quiet behind legal and bureaucratic walls.
Federal and state policymakers should require timely breach notification, with clear explanations and actionable steps for patients. Transparency builds accountability, and without it, reform is nearly impossible.
Funding for Small and Rural Hospitals
Security cannot be a luxury. Policymakers must recognize that underfunded hospitals face disproportionate cybersecurity risks. Small and rural facilities often operate on thin margins, and many lack the staff or infrastructure to implement even the most basic protections.
Federal grants or cost-sharing programs could help bridge this gap. Similar to the funding mechanisms used in education and broadband expansion, hospital cybersecurity grants could fund upgrades for critical access hospitals, community clinics, and nonprofit providers.
This kind of policy would directly address the resource inequality identified in previous sections. Without it, the hospital cybersecurity crisis will remain a story of uneven defenses and preventable harm.
For more on how digital identity policy intersects with hospital network security, see our post on Trump’s repeal of the national digital ID initiative. It highlights how gaps in identity standards also create downstream risks for hospitals and patients alike.
Hospitals, patients, and lawmakers must now align behind a shared goal: proactive defense. Because the threats that lie ahead will be faster, smarter, and more dangerous than anything we have seen so far. Let’s examine what that future might look like.
Conclusion and Future Outlook
Hospital cybersecurity is no longer a behind-the-scenes technical issue. It is a frontline threat to public health, patient safety, and national resilience. The last five years have offered clear evidence of this shift. Attacks have shut down entire health systems, disrupted cancer trials, delayed emergency care, and exposed the personal health information of millions of Americans. From ransomware attacks on hospitals to medical device vulnerabilities, the stakes have grown too high to ignore.
We are now at a critical juncture. Without enforceable national standards, hospitals will continue to respond reactively rather than strategically. HIPAA cannot carry the weight of modern threat environments on its own. Piecemeal improvements, especially in small and rural hospitals, will not be enough to resist increasingly sophisticated adversaries who exploit unpatched software, unsecured vendors, and untrained staff. Investment in hospital network security must become as essential as investments in trauma response or surgical equipment.
The emerging threat landscape is also changing. Generative AI tools now make it possible to automate phishing campaigns, generate convincing fake job candidates, and even design malware that adapts in real time. These capabilities lower the barrier to entry for attackers and increase the speed at which healthcare systems can be compromised. We have already seen how AI-enhanced deception tactics are being used to infiltrate hospital infrastructure. To understand this growing risk, we covered the next wave of invisible attacks in our article on AI-led cyberattacks.
What comes next will require more than just technical upgrades. It will require a cultural shift in how we treat cybersecurity in healthcare. This includes changing how institutions train their staff, how regulators enforce compliance, how vendors are vetted, and how the public is informed. The cost of delay is measured not just in dollars, but in lives.
As the digital threats to hospitals evolve, so too must our response. If this breakdown was useful, subscribe to the Quantum Cyber AI newsletter to stay ahead of the latest threats and policy shifts impacting healthcare cybersecurity. We deliver data-driven, actionable insights every week.
Key Takeaways
- Hospital cybersecurity is under siege, with 92 percent of healthcare organizations reporting a cyberattack in the past year.
- Ransomware attacks on hospitals are not just technical failures; they have delayed surgeries, caused medication errors, and contributed to increased patient mortality.
- Healthcare data breaches continue to rise, with over 167 million Americans affected in recent years due to unencrypted records and poor access controls.
- Medical device vulnerabilities are often overlooked, yet attackers frequently use them as entry points into broader hospital networks.
- Hospital network security is only as strong as its weakest link, including third-party vendors and underfunded rural clinics that lack the resources to defend themselves.
- Without federal standards and enforcement, hospitals will remain reactive, and attackers will keep exploiting predictable gaps in policy and preparedness.
FAQ
Q1: How often do hospitals experience cyberattacks?
As of 2024, 92 percent of U.S. healthcare organizations reported experiencing at least one cyberattack in the prior 12 months.
Q2: Have cyberattacks on hospitals actually caused deaths?
While attribution is complex, studies have shown that ransomware-induced care delays have contributed to increased mortality after cardiac events and emergency disruptions.
Q3: What is the most common cause of breaches in hospitals?
Unpatched software and phishing remain the most common entry points, particularly in systems lacking routine updates or multi-factor authentication.
Q4: Why hasn’t the government enforced stronger cybersecurity standards?
There are proposals in motion, but currently, hospital cybersecurity remains governed by HIPAA and voluntary guidelines that do not account for today’s threat scale or speed.
Q5: Can small hospitals realistically afford better cybersecurity?
Not without targeted assistance. Many small and rural hospitals operate with limited budgets and need federal support or grants to upgrade their infrastructure and train staff effectively.
